VOICE RESTORATION AFTER ILLNESS OR SURGERY
Voice disorders are not limited to “hoarseness after a cold.” They represent a broad spectrum of conditions with different etiologies and mechanisms. In ICD-10, voice disorders are classified as dysphonia (R49.0/R49.1). Dysphonia may occur as an independent condition or as a symptom of benign or malignant laryngeal tumors. Typical manifestations include hoarseness, weak or rough voice, altered pitch and range, and sometimes dyspnea. In severe cases, aphonia develops — a complete loss of phonation with preserved whispering. Dysphonia affects not only communication but also social activity, professional performance, and the patient’s emotional well-being.
Management should always be multidisciplinary, involving ENT specialists, neurologists, and psychotherapists.
Three Main Causes of Voice Disorders
Voice is produced when the vocal folds vibrate under air pressure from the lungs.
The main causes of dysphonia are classified into three groups:
- Organic – structural changes in the larynx or vocal folds (nodules, polyps, cysts, scars, inflammation, tumors).
- Neurological – impaired innervation or muscle activity (recurrent nerve paralysis after surgery, stroke, Parkinson’s disease, multiple sclerosis).
- Functional – no visible structural damage, but impaired voice function. Functional disorders may progress into organic changes over time, leading to nodules or persistent pathology.
“Bad Habits” of the Larynx
Ways to lose your voice quickly include overloading the vocal folds. Shouting, singing, whispering, coughing, attending noisy events, and frequent throat clearing all contribute. Irritating foods and drinks (acidic, salty, fatty foods, caffeine, alcohol) dry and inflame the mucosa. Cold, dry air and noisy environments increase strain. All these factors overload the larynx, leading to hoarseness and potential long-term injury.
Mechanisms of Dysphonia
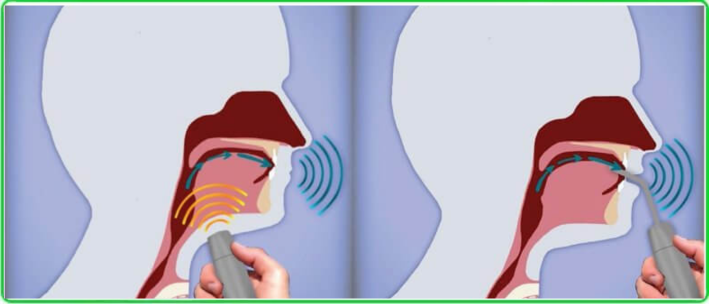
Phonation is a complex neurophysiological process involving:
- The respiratory system (lungs, trachea, bronchi, chest muscles, diaphragm),
- The larynx as the sound generator,
- Resonators (oral, nasal, pharyngeal cavities, paranasal sinuses),
- The central nervous system (motor cortex, cerebellum, cingulate cortex, brainstem).
Voice disorders may develop due to:
- Edema and thickening of the vocal fold mucosa (laryngitis),
- Altered sensory feedback (reflux, infection, strain),
- Muscle tension dysphonia,
- Neural conduction damage (post-surgical or neurological).
Modern fMRI and EEG studies demonstrate altered brain network activity in dysphonia, explaining persistence and relapses.
When to Seek Medical Attention
Voice changes are often overlooked, yet they may be the first and only symptom of laryngeal cancer.
Key red flags:
- Hoarseness >2 weeks, even without pain or fever.
- Recurrent loss of voice or evening fatigue of the voice.
- Sudden hoarseness without clear cause (may indicate vocal fold paresis or nerve injury).
- Dyspnea, stridor, or noisy breathing (edema, glottic stenosis, or paralysis).
- Persistent throat pain or “lump in the throat” (chronic inflammation, reflux, or neoplasm).
- Fever >38 °C, productive cough, or hemoptysis (bacterial or severe airway pathology).
- Heartburn, nocturnal cough, chronic throat irritation (laryngopharyngeal reflux).
- Post-thyroidectomy or laryngeal surgery hoarseness >2–3 weeks (possible recurrent nerve injury or scar).
Why Voice Changes Should Never Be Ignored
Many countries run national screening programs for cancers of visual localizations (skin, lips, oral cavity, pharynx, larynx, breast, cervix, rectum). Core principle: any visible or endoscopically accessible lesion must not be ignored. Every physician — therapist, endocrinologist, gastroenterologist — should ask patients about voice changes. Persistent hoarseness >2–3 weeks requires referral to ENT. This approach reduces advanced laryngeal cancer cases and improves survival and voice preservation.
Natural Methods of Voice Restoration
The larynx is a muscular organ. Like any muscle system, it requires training, rest, and proper care.
- Vocal hygiene: from complete voice rest to regulated use.
- Hydration: warm fluids, saline inhalations, humidified air.
- Diet: avoid alcohol, caffeine, spicy or acidic foods.
Medical Treatment (by ENT Specialist)
Therapy is tailored to etiology:
- Anti-inflammatory and anti-edematous agents (NSAIDs, topical antiseptic sprays, corticosteroids — local or systemic).
- Antibiotics (only for proven bacterial infections, e.g., purulent laryngitis).
- Mucolytics and expectorants — reduce mucus viscosity, improve clearance.
- Antihistamines — in allergic laryngitis or chronic edema.
- Anti-reflux therapy — PPIs, antacids for reflux-related dysphonia.
- Symptomatic agents — analgesics, antipyretics.
- Vitamins and supportive therapy.
Voice Therapy (Phonopedic Rehabilitation)
Conducted by a speech therapist or phoniatrist. Focus: restoring healthy phonation and preventing relapse.
- Breathing: diaphragmatic breathing, prolonged exhalation, breath-speech coordination.
- Phonation: soft voice onset, vowel chanting, humming/vibration exercises.
- Technique: articulation clarity, resonant voice training, rhythm and intonation exercises.
Physiotherapy and Manual Methods
- Manual laryngeal therapy – gentle massage to release neck/laryngeal muscle tension.
- Respiratory exercises – diaphragmatic breathing to reduce vocal strain.
- Physiotherapy – ultrasound, laser, electrostimulation for edema reduction and tissue regeneration.
- Biofeedback (BFB/EMG) – real-time visualization of vocal fold activity to train correct control.
Surgical Management
Indicated for nodules, cysts, polyps, scars, or post-surgical complications.
- Microlaryngosurgery – removal of nodules, cysts, polyps under microscope/endoscope.
- Laser or radiofrequency surgery – minimally invasive, tissue-sparing.
- Injection laryngoplasty – hyaluronic acid, collagen, fat, or implants for vocal fold paresis/atrophy.
- Phonosurgery – procedures to optimize vibratory properties and improve sound quality.
Prevention
- Annual ENT check-ups for high-risk groups.
- Mobile apps (“Voice Health Control,” “VoiceScreen”) allow daily self-tests, acoustic monitoring, dynamic tracking, and reminders for medical visits.
- Particularly useful for teachers, singers, speakers, and post-surgical patients.
Why Patients Recommend KindCare Medical Center
- State-of-the-art diagnostic and therapeutic equipment.
- Individualized voice therapy programs.
- Multidisciplinary teamwork: ENT, neurologist, pediatrician, rehabilitation specialist.
- Minimally invasive interventions and rapid recovery.
- Led by Dr. Maryna Kryshtopava, PhD, Associate Professor, ENT specialist with 23 years of experience. Author and co-author of publications in Journal of Voice, Folia Phoniatrica et Logopaedica and others. Active participant in European scientific conferences with highly cited research in voice disorders. Her mission: not only to treat but to prevent voice disorders — helping teachers, singers, and professionals to preserve a confident and healthy voice.
- At KindCare Medical Center we restore the voice — and protect it for years to come. Book your consultation today for precise diagnostics and modern treatment of voice disorders.