Adenoids in Children: When to Treat and When to Remove
When the grass was greener and doctors were tougher
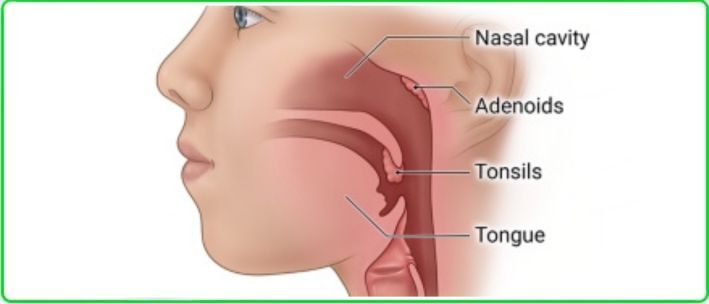
A child is born, takes a breath, and cries! The mission is clear — to live a long and happy life. From the sterile womb, the newborn enters a world filled with viruses, bacteria, and fungi. At first, immunity offers protection. Then the adaptive immune system begins to develop. Adenoids are the first line of defense against these external aggressors.
In the glorious days of Soviet medicine, there was a firmly held belief: if a child’s adenoids were removed, they would catch colds less often. This surgery is called adenoidectomy. Doctors, teachers, and parents alike considered it an almost universal method of strengthening the immune system.
Back then, the procedure was often performed practically without anesthesia — the child would be strapped into a special chair with bandages, and the surgeon would work as quickly as possible. One can only imagine the psychological trauma this practice left in a generation of children.
Today, things have changed. Anesthesia and sedation are now standard, and no one will intentionally subject a child to unnecessary suffering. Still, the debate about whether to remove the tonsils and adenoids “just in case” continues.
Why Doctors Suggest Removing Adenoids and Tonsils
Parents may agree to surgery for various reasons:
- The child frequently has colds, flu, or tonsillitis.
- Nasal breathing is consistently obstructed.
- The child snores, sleeps poorly, and wakes up tired.
- Doctors recommend it as a “prevention” for chronic illnesses.
The core problem is that some physicians still believe removing adenoids improves overall health and reduces the risk of respiratory infections. Furthermore, recurrences of adenoids remain possible even with modern surgical techniques, including procedures performed under visual control. The main drawback of adenoidectomy lies in the very nature of any surgical intervention — it has both advantages and disadvantages, including potential psychological trauma for the child.
This is why alternative treatments for adenoids are continuously being explored.
What Modern Research Shows
European researchers conducted a large-scale analysis of thousands of children who had undergone adenoidectomy, comparing them with those who had not.
The results were surprising for supporters of the “preventive” approach:
- The frequency of doctor visits for respiratory infections did not differ between children with or without adenoids.
- In all children, regardless of surgery, the number of colds naturally decreased with age.
- In adults, no correlation was found between adenoid removal in childhood and the frequency of respiratory illnesses.
In other words — surgery is not a guarantee of good health.
Why “Remove Just in Case” is Not a Good Option
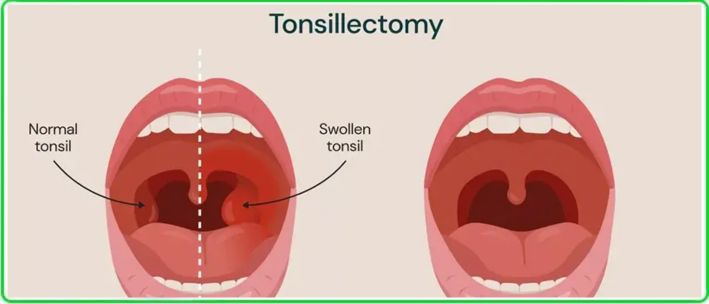
Tonsils and adenoids are part of the immune system. The Waldeyer’s lymphatic ring plays a vital role in protecting the body from infections, especially during childhood. Removing them without strict medical indications deprives the child of a natural barrier against bacteria and viruses.
Moreover, many adults who underwent this surgery as children still remember it negatively. Even though modern procedures are painless, the risk of psychological stress and hospital-related anxiety remains.
When Adenoid Removal is Truly Necessary
There are only three strong medical indications:
- Airway obstruction — adenoids of grade 2 or 3 causing nasal breathing difficulties both day and night, or complete nasal obstruction with episodes of sleep apnea.
- Frequent ear infections with hearing loss — adenoids contributing to Eustachian tube dysfunction.
- Adenoid facies — abnormal development of the jaw and facial bones, along with malocclusion.
Relative indications may include frequent sinus infections, nasal speech (hyponasality), and persistent bad breath.
Bottom Line for Parents
- If your child often gets sick, start with comprehensive diagnostics, not surgery.
- Seek the opinion of experienced physicians — ideally more than one.
- Remember: removing adenoids as a preventive measure against colds is unnecessary.
- Surgery is justified only in cases of serious functional impairment.
In conclusion, adenoids should only be removed when it is a matter of normal breathing and sleep — not for vague “quality of life” improvements. Everything else is a myth that belongs in the past.